Patient Experience Tools
Understand the individual. Delight the masses.
Get to know your patients like never before. See patients from every angle to prioritize and predict their needs. Reduce friction points in the patient journey to build a better experience from start to finish and beyond, from one platform that does it all. Our patient experience management platform is the engine behind precise improvements to the physical and virtual care experience.
How we take you from insight to action
Get the answers you need
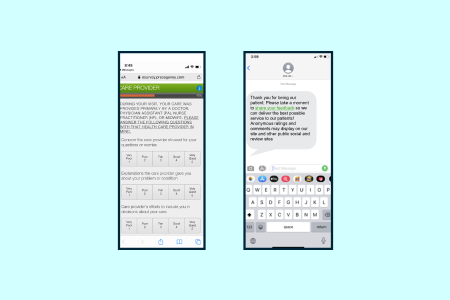
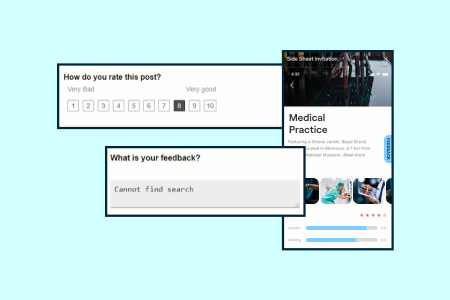
From omnichannel listening to surveys of all sizes, our patient experience tools let you design and deploy bespoke programs to gather patient responses that really mean something.
Pull it all together
Across patient experience surveys, reviews, social media, rounding, and more, we pull all your patient data together and connect the dots.
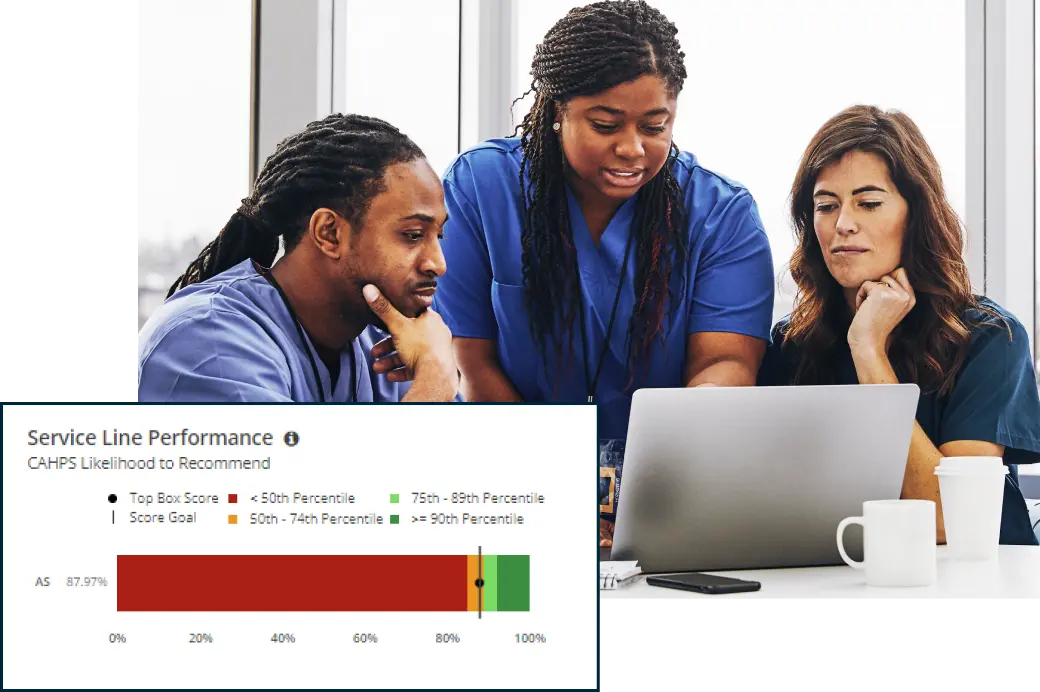
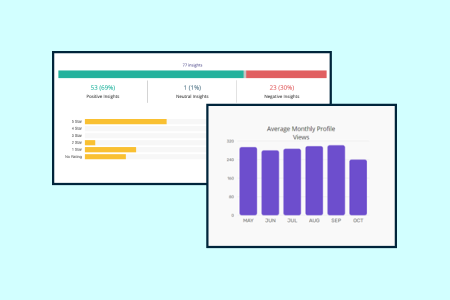
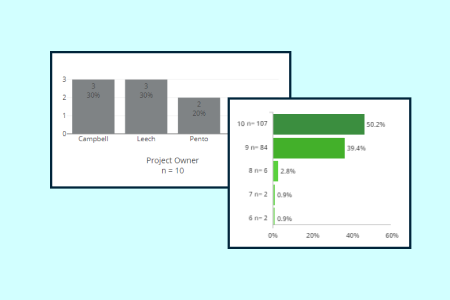
See the stories in your data
With vivid dashboards, AI-powered text analysis, and a suite of other powerful analytics tools, you get a clear read on what’s working for your patients—and what’s not.
A friction-free experience—for you and your patients
Build powerful engagement strategies with flexible, scalable patient experience survey tools that are just as easy for you to create as they are for patients to take.
LEADERS IN PATIENT EXPERIENCE
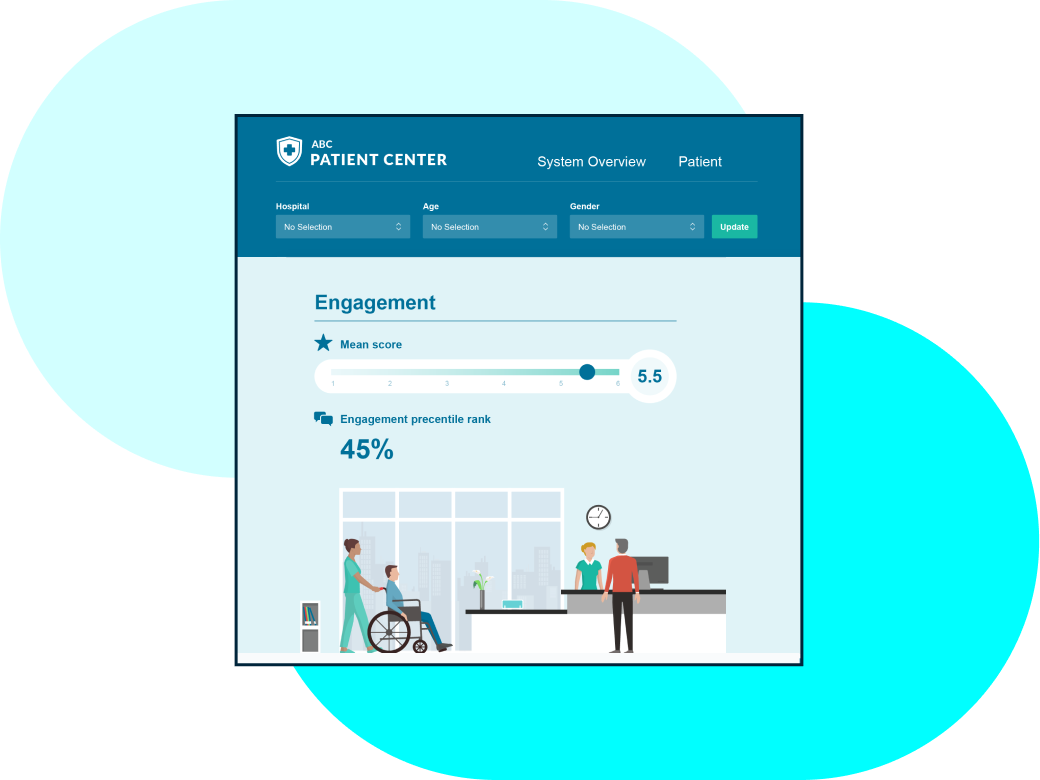
See your patients like never before
Get to know the people you treat—who they are, what they need, and what’s going to win their loyalty. Remix your patient experience data by any metric that matters—hospital, procedure, gender, ethnic identity, and more. And do it all in real time, with patient experience data that flows in and shows up instantly for everyone who needs to see it.

DATA-FUELED DECISIONS
Think beyond the patient experience survey
Our patient experience software gives you a comprehensive picture of the healthcare experience, as told by your patients. Connect with patients in new ways across their journey in virtual focus groups and online communities. Generate fresh ideas from your patients to drive innovation.
COMPETITIVE BENCHMARKS
Biggest datasets. The best benchmarks.
No one has the data we do. See how your patient experience stacks up against the rest of the healthcare sector, set benchmarks that make sense, and draw on knowledge from a galaxy of healthcare providers.
If you know PX,
you know Press Ganey
4/5
Leading hospitals on PX platform
41,000
Hospitals and clinics
1 billion
Patient voices
476M+
Patient touch points annually
PARTNERING WITH THE BEST






Your biggest challenges meet our best patient experience management solutions
Problems we solve
Human Effort Score
gather
Continuous listening
gather
Digital feedback
visualize
Interactive dashboards
“Modernizing and digitalizing our surveys was an easy decision, because it’s allowed us to reach more patients in real time.”
Dr. Mark Kerschner
Medical Director, Bronson Methodist Hospital Emergency Department, Level 1 Trauma Center
Patient Experience Software
A patient experience that builds love and loyalty
Get in touch, and we’ll show you how our patient experience software makes it easy to deliver great PX, every time.