
HX Insights
The evolving expectations of today’s healthcare consumer
In 2023, Press Ganey national data revealed a consistent uptick in patients’ rating of experiences in acute inpatient care, almost completely reversing the downturn seen between 2020 and 2022. While patient experience in emergency departments continues to be a challenge for many healthcare systems, we’re beginning to see promising improvements in that area as well.
Leading health systems saw the benefit of offering flexible options for getting care during the pandemic—meeting demand by shifting volume to lower-intensity settings and modalities. Many have matured those COVID-stopgap measures, integrating them into their access strategies and establishing new access points for on-demand care via telehealth services and partnerships with retail providers and/or stand-alone urgent care providers.
Unlike acute care, medical practices sustained high performance, with “Likelihood to Recommend” (LTR) increasing during the pandemic. This reaffirms the patient-physician relationship as the cornerstone for care, which is an important consideration for evolving healthcare models and strategies. Establishing a trust-based relationship will always be a prerequisite for patient satisfaction and enduring loyalty.
However, it’s clear that consumer expectations in healthcare are rapidly evolving. The convenience, simplicity, and personalized experiences enabled by technology in other aspects of our lives have led consumers to expect similar experiences in healthcare. This shift in consumer expectations is reflected in how people go about choosing a doctor.
A recent Press Ganey consumer survey reveals a growing trend among consumers to conduct online research when choosing a doctor, with 37% of respondents indicating they now find their doctors online. In fact, 2023 marked the first year the internet became more important for choosing a doctor than referrals from friends, family, or another physician. Moreover, consumers are consulting multiple websites and reading multiple reviews before choosing a doctor. Significantly, 84% of respondents stated they would not consider a physician rated less than 4 stars.
This shift in consumer behavior underscores the need for healthcare providers to adapt to meet new consumer expectations in healthcare by making performance ratings accessible, leveraging technology to enhance the patient experience, and focusing on earning and re-earning the trust and confidence of their patients with every encounter, across the full spectrum of encounters.
Drivers of patient trust and confidence
We see further evidence of evolving consumer expectations in healthcare when analyzing the impact of friction on patients’ willingness to recommend a medical practice. When a patient experiences friction at any time, it erodes their trust in their provider and the practice. Friction can occur before, during, or after care—in the form of challenges contacting the practice, getting an appointment, wait times, availability of lab results and other pertinent medical records, or receiving post-visit follow-up from the practice.
Patients who respond favorably to questions about these aspects of their care are highly likely to recommend the practice (99th percentile results). Conversely, any amount of friction erodes patients’ “Likelihood to Recommend”—and the magnitude of friction experienced has a corresponding negative effect on “Likelihood to Recommend”.
Clinicians often interpret low relative performance on patient experience scores as a critique of their bedside manner, yet the friction data reveals a different message: Suboptimal workflows and care processes torpedo the scores of even the most compassionate, skilled, and dedicated clinicians. Friction in the patients’ care journey erodes trust in the system and confidence in the medical practice. Eliminating friction and improving coordination builds trust with the medical practice and the care they provide.
Patients’ heightened awareness of safety
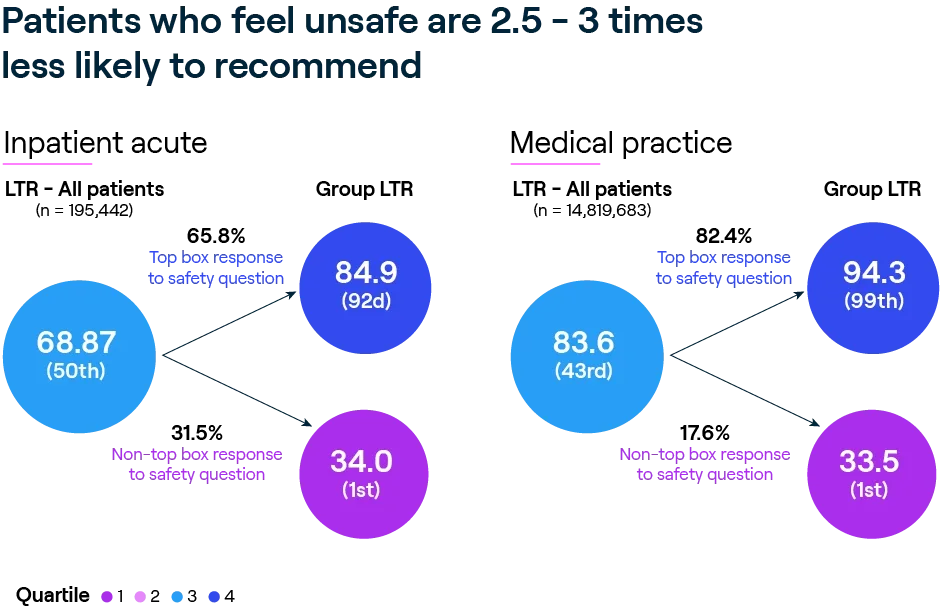
COVID taught patients to be alert to their safety in care environments, and we see the impact of patients’ perception of safety is showing up in their responses to the “Likelihood to Recommend” question. Our analysis of more than 12 million responses to ambulatory care surveys reveals that patients who give an unfavorable response to questions about whether staff provided care in a safe and secure manner are 2.5–3x less likely to recommend the hospital or medical practice.
Consistent with contemporary definitions of harm, patients’ perception of safety extends beyond their physical safety to include interactions that contribute to emotional security or harm. Using natural language processing (NLP) to analyze survey comments, we find that patients describe experiences of feeling safe (or unsafe) in terms of feeling respected (or disrespected) in the way their caregiver communicated with them, through behaviors like how patiently next steps in the treatment are explained, being attentive to concerns, and giving thorough answers in a friendly manner to questions about safety.
Patient-provider interaction
Provider and staff interactions with patients do matter, especially in an environment where consumers have greater expectations and a heightened sensitivity to safety. Our analysis of 12 million patient responses to medical practice surveys shows that responses to questions on confidence in the provider’s skills, evidence of teamwork among members of the care team, demonstrated compassion for the patient (they are listened to; the provider demonstrates concern for their worries), and shared decision-making are powerful predictors of patients’ “Likelihood to Recommend” the practice. When care teams demonstrate all four attributes—providing care that inspires confidence, acting with coordination, and being visibly compassionate—99% of patients recommend the medical practice.
The loyalty impact of interactions between patients and the people involved in their care holds true across settings, with minor nuances. Regardless of where care is received, patients’ assessment of how they were treated—feeling respected, listened to, communicated with, included in decision-making—shapes their confidence in the system and the people caring for them.
Patient Journey
Implications and opportunities
Rising consumer expectations in healthcare and the proliferation of new options for care adds imperative to accelerate care redesign. Health systems are leaning into this work, committing to finally and truly organizing around the needs of patients, with the goal of reducing complexity, tailoring care to the individual, and optimizing the patient experience.
The range of initiatives includes strengthening the digital front door, shifting more care to outpatient settings, partnering with other providers to improve access, establishing hospital-at-home services, investing in artificial intelligence (AI), and more.


flexible methods
Starting now, make healthcare easier
Reducing complexity where possible is key to building patient confidence and earning loyalty. Understanding where friction occurs in the patient’s journey is essential to solve the right problems. The work extends beyond traditional post-care surveys. To understand where the experience can be optimized, health systems need to gather feedback and input using dynamic and flexible methods. Leading systems are supplementing surveys with language analytics, digital focus groups, and electronic communities to really understand patient expectations and priorities.
Real-time, omnichannel listening
Continuous listening systems provide service recovery alerts to resolve individual issues and shine a light on system failures that require process redesign (e.g., wait times and poor care coordination) or service failures that indicate a need for training and coaching (e.g., communication skills and service behaviors). New capture modes, such as in-app or in-care feedback, and point-of-service QR codes complement traditional post-care surveys and identify additional sources of friction. Digital surveys designed specifically to measure the Human Effort Score sharpen focus and execution.
Artificial intelligence derived from NLP
Patient survey comments and other unstructured texts are a rich source of information, offering nuance to quantitative results. AI spots emerging themes that are difficult to replicate by human review, due to the sheer volume of comments. The results enable service recovery, offer healthcare consumer insights on the experience of new care models, and inform care redesign efforts.
Invite patient input at scale
Patients are often willing—and eager—to provide input to make care better, but health systems struggle to capture input representative of their full populations. New digital capabilities enable provider organizations to broaden their reach and invite input at scale. Virtual PX design sessions, digital patient panels, and digital communities open the aperture for input with synchronous and asynchronous models convenient and available to all members of the communities they serve.
CX/PX strategy
Focus on the digital front door
High-performing organizations recognize that, today, the trust continuum begins online. In response, they bring diverse colleagues to the table to design the consumer experience (CX), reflecting an integrated CX/PX strategy. Together, the chief marketing officer, chief experience officer, and care delivery leadership are collaborating to ease the way for patients by focusing on key touchpoints and making relevant information available to consumers:

- Ensure provider directory information is complete and current to reduce friction.
- Publish patient experience ratings and comments in physician directories to aid research and decision-making, and to build trust through transparency.
- Publishing ratings and comments to third-party listings sites. Publishing to third-party sites offers the dual benefit of providing relevant information to consumers no matter where they research their options, while ensuring the information on those sites is derived from validated surveys and is representative.
Segment performance results to identify gaps
While best practices and high reliability principles offer the surest way to optimize the system, it remains essential to understand the unique needs of patients. There are important differences in how patients experience and evaluate care based on their health status, care needs, age, gender expression, and race or ethnic backgrounds. Leading health systems address variation by looking for it, then evaluating whether best practices or friction have an equal impact for all groups.
- Segment patient experience results by patient attributes—both quantitative results and AI analysis of unstructured text.
- Use key driver analysis to determine if key drivers are equally impacting all groups.
- Invite input from groups experiencing gaps using digital and virtual engagement modes, such as virtual PX design sessions and digital patient panels.
high reliability
Leverage HRO practices
HRO principles and practices are routinely thought of as foundations for safety and quality, but not routinely considered as the basis for consistently excellent experience of care. In studying organizations that have performed in the 90th percentile consistently for two years, three high reliability practices emerge.

- Established behavior standards: These are articulated and modeled at every level in the organization. In many cases, these standards have evolved from first-generation service behaviors (e.g., walking patients to their destination, eye contact) to universal relationship and reliability skills that promote patient and colleague relationships.
- Promote teaming through daily huddles: The practice of team huddles in both clinical and nonclinical areas improves the employee experience and is foundational to consistently delivering a coordinated team experience to achieve optimal outcomes and experience.
- Structured leader rounding initiatives: These include rounding on both patients and caregivers. Rounding initiatives ensure that leaders have the structure and process to connect consistently with patients and their teams. Rounding provides routine opportunities to model behaviors, give positive feedback and provide coaching, and demonstrate leaders’ commitment to promoting safe, high-quality, compassionate care—as well as engaging caregivers to deliver that care.
Future-proofing the patient journey: The patient experience, care innovation, and high reliability organizing
Increasingly complex care is moving outside the walls of hospitals, allowing for excellent clinical outcomes in a more personalized, compassionate, and convenient way. Leading organizations are focused on innovating and rapidly iterating toward minimally disruptive medicine—care pathways that reduce the suffering of patients, simplify the journey, and facilitate coordination among providers and caregivers. Moving quickly to integrate innovations into daily work, once they are proven to meet their objectives, is key. When it comes to innovating effectively and safely, then translating innovation pilots into practice, HRO competencies act as an accelerant.
Organizations that have adopted HRO principles will recognize how they serve as a chassis for innovation. Transformation through organizational learning is at the heart of HRO. In studying Press Ganey client performance before, during, and following the pandemic, we observed that organizations that fully embrace HRO principles and practices were more resilient across all performance domains to both the initial and trailing effects of COVID. Hardwired HRO competencies enabled them to respond more rapidly through reliability-based learning, adaptation, and innovation.
On top of committing to best practices, HRO involves wrapping around those best practices the competencies that ensure ongoing organizational learning and best practices sustainment—essential elements for improvement and transformation. The very same skills that help organizations reduce variation and improve outcomes serve as a disciplined process and framework for intelligent risk-taking—exploring and trying new ideas that enable transformation.
The essential people competencies of HRO
- Relationship skills, to foster collegiality and empathy, with an emphasis on moderating the power distance and the authority gradient, and deferring to expertise.
- Reliability skills, to engender a preoccupation with failure among staff, with the objective of reducing the incidence of human errors and mistakes that lead to failure.
- HRO leader skills, to ensure alignment on mission, build accountability, prioritize and solve problems, ask questions to anticipate and avoid events, and commit to being a learning organization.
HRO principles reduce variation and spur innovation*
- Sensitivity to operations: Understanding that front-line staff members are best positioned to identify opportunities for improvement and the ways to address them. Routinely incorporating their input into design. Leveraging operating data to fuel understanding and expose gaps.
- Deference to expertise: Putting knowledge above authority and encouraging all people to speak up when they notice a problem or have an idea that could eliminate friction and lead to improvement.
* K Weick & K. Sutcliffe, Managing the Unexpected: Assuring High Performance in an Age of Complexity
- Reluctance to simplify: A commitment and discipline to seek full explanations of complex situations instead of relying on superficial understanding.
- Preoccupation with failure: Thinking through all possible sources of harm and scenarios where it could occur, or that might cause the objective to be missed. Spotting and responding to failure quickly when it does occur.
- Commitment to resilience: Rapidly assessing and responding to challenges to achieve recovery.
HX Insights
Let’s innovate the future, together
To learn how Press Ganey’s Human Experience platform can support your organization’s transformation, reach out to our team.
