
HX Insights
Building a thriving healthcare workforce
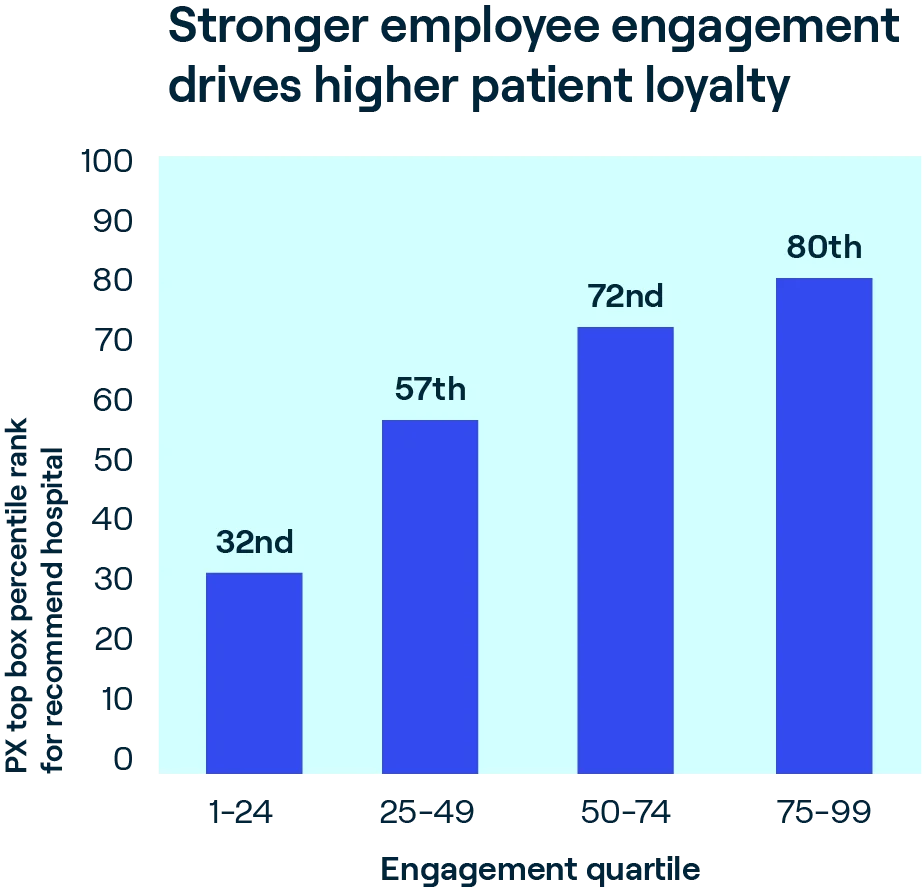
At the heart of great healthcare are the physicians and caregivers dedicated to delivering safe, high-quality, patient-centered outcomes. Efforts to build social capital by nurturing their dedication through engagement strategies create a powerful flywheel effect: Year over year, our data shows the strong association of employee engagement with patient experience, safety, and quality of care.
Press Ganey national data, based on responses from 1.4 million employees across 4,000 provider organizations, shows signs that workforce engagement is stabilizing after a multiyear downward trend that began prior to the pandemic. Yet despite these gains, and the inherent rewards of a career in healthcare, many organizations are hard-pressed to attract and retain skilled staff. Addressing workforce issues continues to be the #1 priority among health system CEOs, given current and expected labor shortages.
Underlying the aggregate data is a large gap in engagement between top and bottom performers—a gap that has widened over the last three years. The top decile of performance is now higher than it was before COVID hit, while bottom-decile performance is worse. Important lessons emerge from both ends of the curve—and clear evidence that, with the right approach, it is possible to improve engagement in today’s challenging environment.
Average scores on engagement and intent to remain differ significantly by role, with the lowest scores concentrated among front-line caregivers. Despite modest gains in 2023, nurses, APPs, licensed technical staff, and physicians are consistently at the low end of the engagement curve each year.
This means the highly skilled people who interact with patients on a daily basis struggle to stay connected to their work and achieve professional fulfillment. And they’re at the highest risk of leaving.
Organizations diagnosing their own opportunities for improving engagement will benefit from looking at performance and performance drivers at different units of analysis—including role, team or work unit, shift, gender, and tenure—to home in on their precise opportunities and next best actions.
Where to focus: Drivers of physician and caregiver engagement
Sustaining high performance on caregiver and provider experience is no accident. A key driver analysis of organizations that have maintained high engagement despite the industry’s macro pressures reveals common strengths, as perceived by their caregivers and providers.
These center on themes of respect, senior management behavior and actions, and commitment to quality and safety—all key facets of trust and social capital. Notably, while compensation and staffing are correlated to engagement, they are not among the top 10 drivers of engagement. Fair pay and adequate staffing are table stakes, but they’re not among the aspects of workforce experience that drive engagement and contribute to the creation of social capital.
Top 10 drivers of employee engagement
1
Treating employees with respect
2
Senior management’s actions support the organization’s mission and values
3
A commitment to quality improvement
4
Conducting business in an ethical manner
5
Employees’ perspectives factored into decision-making
6
The organization’s work climate promotes patient safety
7
Confidence in senior management’s leadership
8
Satisfaction with job security
9
Caring about customers
10
Caring about employee safety
Safety first
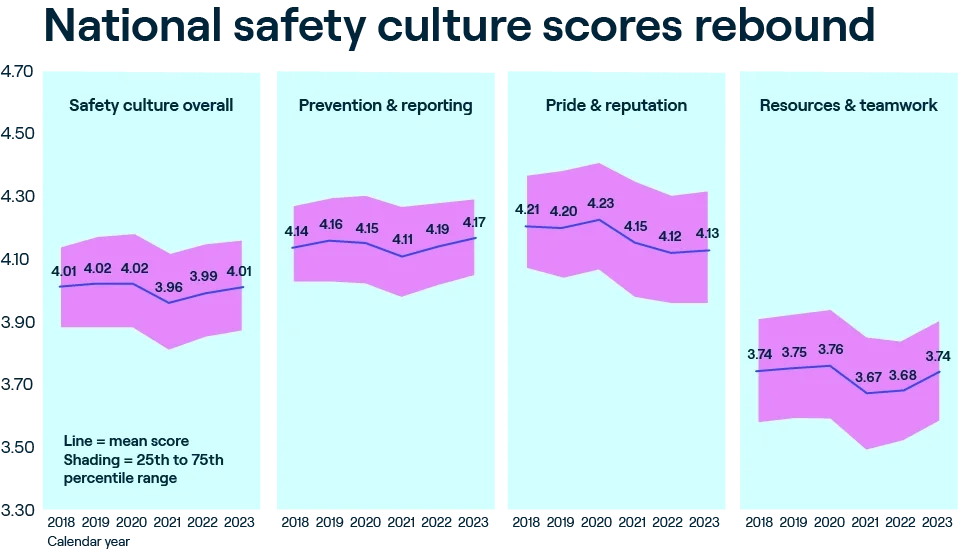
Top-performing healthcare organizations put safety first. This commitment is crucial for patient care as well as for building a sense of pride and motivation among staff. There is a strong positive correlation between safety culture scores and employee engagement—and the magnitude of the correlation has intensified since the start of the pandemic. Annual results from Press Ganey’s safety culture survey, the most widely used in the U.S. with feedback from nearly 1.4 million healthcare workers a year, confirm this pattern.
Safety culture is reported as a composite score, but the correlations between engagement and the subscales—resources and teamwork, prevention and reporting, and pride and reputation—illustrate powerful relationships. Simply put, when a healthcare organization prioritizes safety by fostering a culture of safety, its employees are more able to be fully invested in their work.
Prior to the pandemic, national aggregate safety culture scores were on the rise—and safety events were on the decline. But the stress of COVID on the healthcare system eroded national performance across all measures. In 2021, organizations redoubled efforts around safety, and results in 2022 brought gains in the prevention and reporting subscale, followed by gains across all subscales in 2023.
Notably, it is among employees in front-line roles where we saw the greatest improvement in perception on questions related to resources and teamwork and prevention and reporting. Safety culture is a rising tide measure: Organizations that continue to invest in this area will realize gains across patient, caregiver, and business outcomes.
Organizations with the strongest safety cultures have multiple attributes and practices in common. These include highly visible leadership, tiered safety huddles, leader rounding, transparency around issue identification and resolution, and high reliability communication behaviors for leaders, managers, and front-line staff. They also involve front-line staff in improvement initiatives—with the dual benefit of faster improvement cycle time and fostering better engagement.
Drivers of retention
Retaining the skilled people we recruit is a universal priority, yet it’s getting harder to do. An examination of employee census data from health systems and hospitals that survey annually with Press Ganey reveals that between 2022 and 2023, one in five healthcare employees left their organization—a rate that increases to one in four for employees with less than two years’ tenure.

Additionally, at the role level, we see similar patterns for turnover to those we saw in engagement: greater turnover risk among certain front-line employees. The compounding effect of tenure on new front-line employees, who are already at greater risk for leaving, underscores the importance of onboarding efforts that extend well beyond orientation.
But encouragingly, strong leader-employee relationships reduce turnover risk: Teams with high leader index scores had an average turnover rate of 16% vs. teams with low leader index scores, which saw 23% of employees depart.
Analysis of survey results shows the critical impact of organizational culture on engagement and retention: In addition to a commitment to safety, equity, respect, and a sense of belonging are highly correlated with employee retention across all roles. And they have a well-understood link to safety outcomes: If staff members don’t feel respected, valued, and included, they are less inclined to speak up and raise concerns, putting patients and the organization at substantial risk.
Key driver analysis reveals nurses are more likely to stay with an organization when they feel a strong sense of inclusion and belonging and believe their job is the right fit for them. For physicians, feeling aligned with their organization—having respectful relationships with leadership, being part of decision-making processes, and sharing a common vision for the organization’s mission—plays a significant role in retention and engagement.
Our workforce engagement research reveals common approaches and practices among top performers. In addition to hardwiring the leadership behaviors that improve safety and reliability, top performers keep their fingers on the pulse of their workforce. They complement annual engagement surveys with an omnichannel, continuous listening strategy to allow for rapid surfacing of and response to pressing issues—helping to reduce friction and distractions experienced by staff to enable top-of-license practice and professional fulfillment.


Implications and opportunities
Attracting and retaining top talent is not a new priority for health systems. But the competitive labor market, coupled with a labor shortage that will persist into the future, mandates new approaches to the work. The healthcare workforce is under different pressures today than it was even just five years ago; employees’ needs and expectations have changed. Leading organizations are revamping their employee value proposition and talent management strategies in response.
Immediate work to address pressing needs
Leading health systems are focusing efforts on dual priority areas: meeting the immediate needs to retain, attract, support, and develop talent, and laying the groundwork to transition to and support care models of the future. Taking these actions is tantamount to making a down payment on building the social capital and trust organizations need to thrive in today’s challenging environment.
Onboarding: Modern onboarding programs recognize that building engagement starts on day one. Unlike orientation programs, robust onboarding programs focus on connecting new employees to the organization more broadly—its mission, vision, and values—to their unit or department, and, finally, to ongoing opportunities for their own professional development. Fostering a sense of belonging is key to success.
Front-line leader development: Nurse managers are the linchpins of inpatient acute care, but they often don’t get adequate training for the role. A standard, enterprise approach to leader development and coaching yields significant ROI, including higher nurse engagement, improved resilience among nurse managers, reduced nurse turnover, better clinical outcomes, and productivity.
Safety as a core value: Organizations that commit to zero harm and high reliability organizing (HRO) principles achieve gains in employee and patient safety—including psychological safety. In a period of transformation, leading health systems make it a priority to review, refresh, and recommit to enterprise behavior standards, as well as reconfirm mechanisms for accountability, learning, and improvement. They are paying close attention to safety culture, with a particular focus on violence and incivility experienced by caregivers.
Fix broken systems: A poor workforce experience is frequently due to inefficient systems and processes. Lasting solutions come from listening to front-line employees, whose direct experience provides essential insights. When these employees feel their voices are valued and understood, they’re more inclined to consistently offer useful feedback, fostering a positive feedback loop. To gather employee insights on a larger scale, top organizations are turning to innovative technologies, including AI-powered platforms, virtual focus groups, and crowdsourcing.
Future-proofing the workforce: The straightforward, but hard, work of cultural transformation
Change is constant in healthcare. And organizational culture ultimately determines which organizations weather the storm and emerge stronger following major change efforts. Culture is how values are expressed through formal elements of strategy, priorities, and policies, as well as through informal aspects of customs and behaviors. Organizations on the leading edge of the engagement curve have certain things in common across the formal and informal elements of culture. They are: an environment that fosters respect, inclusion, and safety; a commitment to consistently executing on best practices; and a willingness to redesign the work being done. These traits emerge in three principal areas:
1. Committed and involved senior leadership
Employees have confidence and trust in senior leadership. Senior leaders embody the organization’s mission and values in both word and deed—they lead the way with their own everyday behavior and actions. They are highly visible and clearly articulate the organization’s vision and strategy. They embrace transparency to build trust, foster accountability, and ensure a sense of belonging.


2. Established values and behavior standards
Employees feel the organization treats them respectfully. They also feel the organization seeks their feedback to pinpoint opportunities for improvement, as well as their input on just how to improve. Employees and physicians are aligned with senior leadership, and everyone is working toward the same goals. Importantly, there is accountability to abide by the organization’s values, and a method for remediation if people fall short.
3. Adopting high reliability organizing principles
HRO is usually thought of as an approach to achieving safe care and safe practice environments. But the true definition of HRO is “performing as intended consistently over time”—which is relevant in every aspect of care delivery. Adopting high reliability principles and practices can impact all performance domains—including workforce engagement and patient experience. The fundamental principles of HRO—which center around transparency, communication, expertise, and continuous learning and improvement—enable leaders to align mindsets and actions, reduce variation and barriers to great care, optimize processes, and empower people at every level of the organization.

HX Insights
Let’s innovate the future, together
To learn how Press Ganey’s Human Experience platform can support your organization’s transformation, reach out to our team.
